This afternoon I joined another new patient clinic. To be in the role of the examiner is a good change to prepared for my CCAs as I focus during this process on the required points for the final CCAs. Afterwards we sat together and discussed the feedback.We got some very useful advice from our tutor. For instance that we should place the case history by the side when presenting as this really helps us to focus and summarise the main points. But also that we should try to gather more information before we write it down otherwise when we stop for each section we would interrupt or communication and with this the flow of the case history. I really appreciated our feedback session afterwards and keep some spare copies of the new patient feedback sheet so that I can ask an observing colleague for feedback on my performance.
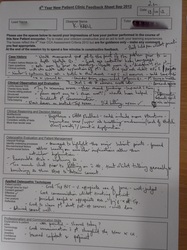
Today I got the promised feedback from last weeks new patient clinic. My tutor mentioned that I used a small amount of open questions, which would be good to do next time as this gives the patient the change to explore details more form their point of view. However we came to the conclusion that in this case it was a good choice as my patient would otherwise have 'taken over' the whole process. Even when I used closed questions and asked sharp questions it was hard to interrupt the patients reports. All in all, I got a very good feedback with hardly any comments. I will add this feedback form to my clinic file and will follow my progress during the year whilst I copy more of those feedback sheets and plan to ask observers that come with my on the day to fill in a sheet.
Today SL, one of my team 2 colleagues, was scheduled to give us a tutorial on the principles and effects of different treatment modalities but due to new patient clinic this was cancelled. Instead I joined a colleague during his new patient clinic as an observer. During the case history I noticed how seldom I actually can join new case histories from my fellow students due to time constrain. However this would be very helpful at this stage. Me and the observing tutor followed the case history process and filled out the '4th Year New Patient Clinic Feedback Sheet'. I really appreciated to take part in this process as our CCAs will mimic this situation. Afterwards we discussed altogether our strengths and weaknesses.
The feedback I gave to my colleague towards the overall case history that the timing needs to be worked on. I agree that in this patient it was better to choose open questions to get full detailed answers but this lead to a delay from early on during the process. Lifestyle issues were considered and noted but not detailed enough. For instance did the patient enjoys doing exercise classes, this was noted but not further explored. The patient gave hints but I could feel was not confident enough to explore it more in detail as he was not sure if this is relevant. For the next point on the assessment sheet I noted that a clear and structured assessment routine is essential. I nearly wanted to step in when my colleague forgot to do an active spinal movement assessment and also did the general observation of the standing/sitting posture got lost. Considering clinical reasoning and choosing the most valid tests I mentioned during our feedback discussion that a neurologic examination would be an essential step when a patient presents with pins and needles but also loss of sensation in the lower extremity. I can understand that this formative assessment is very stressful but all those mentioned points are necessary to make the clinical working diagnosis. At the end of the appointment the patient asked if he is 'treatable' and if we could help him. By that point it was not made clear to him what he was diagnosed with and if osteopathic care would benefit him with his symptoms. I think it is essential to explain all our patients in a clear way what we think is causing the pain and how we consider to treat them, thats the right of a patient. This morning I had my new patient clinic.This clinic allows us to get more feedback on our current clinical performance and prepares us for our final CCAs. It was different from the normal case history taking process as a tutor was present during the whole time but also two observers. All three filled a feedback sheet during my case history and assessed me. This was giving me quite a bit of pressure. I had a lovely female patient who never experienced osteopathy before.
I was quite nervous when we went outside to discuss my hypotheses. However, my tutor and my colleagues were quite happy with my performance so far. I carried on with the examination and also did quite a fair amount of treatment. All in all I was pleased how it all ran. Afterwards I got feedback from all three observers. This was a great experience as I will use this criticism to develop my clinical skills. I was criticised that I ask to many questions in detail for a patient's general health that are not relevant to the presenting symptoms. By today, I always asked quite in depth for those details as I often get some relevant details even if the patient seems to be healthy and gave me the impression to be fine. However I learned from todays' assessment that I have to concentrate on the most relevant details applying my clinical knowledge. So that I consider differential diagnosis with symptoms that could come together with system health features. Another area I need to work on is time management. Although today it went well but my tutor suggested to speed up my process, e g. that I use an alarm, as students are likely to overrun during CCAs. I was so happy to hear that my English communication skills improved, however I need to improve still on this. Therefore I plan to practice the case history taking process in my study group. This will allow me to work on my questioning, communication skills, time management and assessment routine. As there was not enough time this morning I was promised to get further written feedback from my observers next wednesday. This morning I had my patient from last week again. She improved slightly however he symtoms moved now to her left lower back. She pointed towards her left SIJ. I could not reproduce pain on sacral springing, gapping and shearing. I explained my tutor that she now has an iritated left SIJ. We had a disscussion afterwards and I understand now that if I can not reproduce the symptoms on passive assessment it is unlikely that the symptoms come from her SIJ. This patient was the one I discovered last week that it is necessary for whatever reason to assess the spine passively from both sides in the sidelying position. Therefore I did so this time also did I asked my patient to walk up and down in the treatment room to assess her gait. I learnt on saturday when I visited The Three Clinic, to listen to patients more carefully. Her symptoms are aggreviated by walking therefore it is important to examine the gait. When I had finished my treatment I reassessed the gait and the patient felt less achy!!! I look forward when she is coming back, hopefully feeling even better than this time...
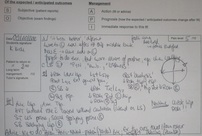
During our clinic tutorial this afternoon we made a plan which topics we would like to cover until our first CCAs in November. Therefore we split out topics and made a plan:
I had a new patient with central lower back pain today. I took the case history, presented to our tutor in the team point and we agreed that I need to assess the patients' lumber spine as well as the SIJ joints. I examined the patient actively and then passively in the side-lying position on the plinth. I assessed a decreased range of movement in the T2-3, L4-5 and LS segments. When the tutor came, she assessed as well the mobility of my patient's spine. In comparison to my examination, the tutor assessed the lumber and lower thoracic spine of my patient from both sides therefore asking my patient to turn to the other side-lying position. At first the tutor disagreed with my findings but then palpated the same findings on the side I had assessed. By that time I never came across that there could be a difference when assessing both sides. Therefore for my future clinical examination I will assess my patients' spine from both sides in the side-lying position.
|





 RSS Feed
RSS Feed